This is not my typical newsletter. It is an update on the health of my family and what we have been going through over the last almost three months. I originally wrote it as a way for me to process what was happening and so I wouldn’t forget where we started and how far we have come. I was encouraged to share this with you all, so here it is!
Having a baby is joyful, wonderful, fulfilling, and amazing. It’s also hard. Adding a second child to the family can be even harder. I expected this. I expected my relationship with L (27 months) to be different, but I was also excited to see her become a big sister. She is a wonderful big sister. I expected to get almost no sleep and there to be a period of rough transition. I also expected so much love, joy, quiet moments, and loud ones too. So far, I have experienced all of these things. We also have been experiencing something so unexpected and so unbelievably difficult.
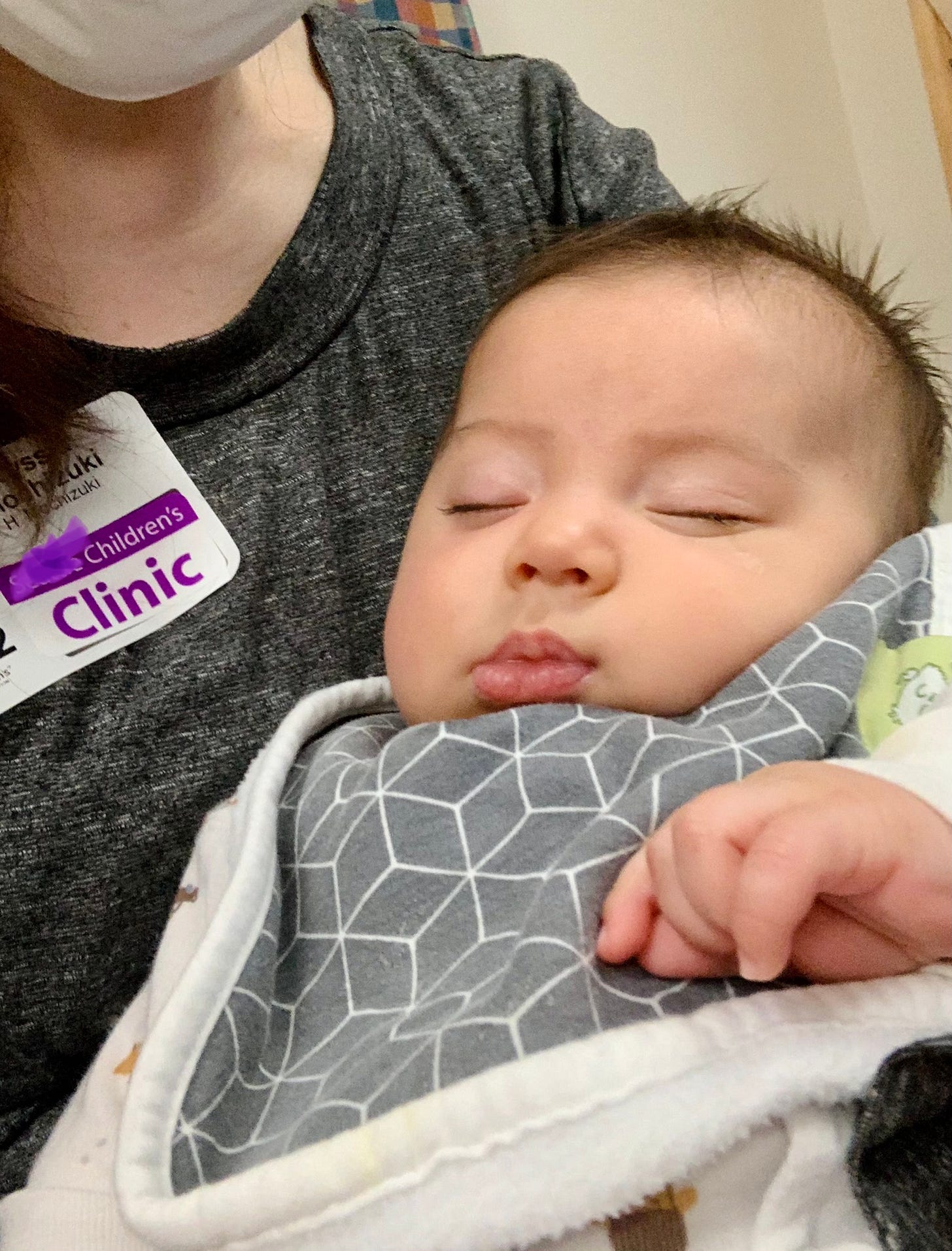
My labor and delivery and the first week or so after were perfect. I couldn’t have asked for a more perfect birth experience. H was doing well too. He was slow to gain weight but seemed to take to nursing easily, he slept well, and rarely cried.
Choking and Coughing
When he was around two weeks old, he started choking and coughing while eating. I saw a lactation consultant thinking he was probably just getting too much milk too fast. She checked him for tongue ties and found nothing. She agreed it was probably just too fast flowing milk. His coughing and choking continued to get worse and he would sound congested after eating. He also started spitting up and vomiting after eating (much more than a normal baby).
Diagnosis: Laryngomalacia
I finally took him in to the pediatrician at three weeks old. She watched me feed him and watched him choke and cough. She listened to his breathing and watched him breathe. She said that she is 95% sure he had Laryngomalacia and reflux. He noted his stridor (high pitched sound on inhale) as a key indicator along with chest and neck retractions which indicated he was struggling to breathe. These along with the choking and trouble eating pointed her to Laryngomalacia.
She told me that Laryngomalacia is a congenital deformity of the larynx that causes an extra flap of tissue to cover the airway. She explained that Laryngomalacia caused noisy breathing (stridor) and was not a cause for concern in most babies. Most babies grow out of it by two years old without treatment. Most babies. She explained that due to the symptoms H was having, it was likely that he had a more severe case. He definitely needed reflux meds (GERD is extremely common in babies with Laryngomalacia and exasperates the condition), but she wasn’t sure he would need much treatment beyond that. She told me that the bad news was that it would get worse before it got better. She wasn’t sure how much worse and it would probably peak around 6-9 months.
However, not all babies grow out of it and some require surgery if the complications caused by Laryngomalacia outweigh the risks of the surgery (supraglottoplasty).
She explained that he will need to be watched carefully and not be on his back for too long. She also told me that it was really dangerous if he even caught a cold and we should take him to the doctor at the first sign of illness.
She immediately started him on reflux medication and gave us a referral to a Speech and Language Pathologist for feeding therapy and a wedge for him to sleep on.
Speech and Language Pathologist Feeding Therapy
The referral took time to come through. In the week after that appointment H got worse and worse quite quickly. He was constantly gasping and grunting in his sleep. I witnessed him stop breathing, gasp, and then cry multiple times throughout the night. There is nothing scarier than watching your newborn stop breathing. He wasn’t sleeping and I wasn’t sleeping either in case he stopped breathing. His stridor was constant, and his reflux was unbearable. He was constantly uncomfortable, constantly spitting up, and always fussy. He was having almost constant retractions at his chest and neck. His oxygen saturation while eating and sleeping was consistently low.
Our pediatrician decided to rush our referral to the SLP to see us as soon as possible. She also referred us to a pediatric otolaryngologist at the children’s hospital to confirm the diagnosis and start treatment there.
We got a call to start feeding therapy the very next day after our appointment where our pediatrician decided he needed a rush referral. I wasn’t sure what to expect and wasn’t exactly sure what they would be able to do for us. At that time, I was much more concerned about his breathing than his eating and was eager to see the otolaryngologist.
Honestly, the Speech and Language Pathologist we saw was not great. It was almost immediately clear that she hadn’t read what the referral was for or what our pediatrician’s concerns were. She didn’t mention anything about a wedge for sleeping or suggest anyway to manage his reflux (which is what the referral was for). I was disappointed and frustrated.
Instead she had us doing oral motor training and finding ways for H to manage my fast flow to reduce the choking. I knew this was not the cause of his choking, or at least wasn’t the root cause. She did note that when he choked it sounded like he was aspirating.
At our second session, she finally measured H for a sleeping wedge. She also finally realized that he had a very uncoordinated suck-swallow-breathe pattern. He also had a weak suck. He would not take a pacifier or a bottle no matter what she (or us) tried. Most of the next few sessions centered around trying to get him to take a bottle and pacifier. Very unsuccessfully.
The Sleeping Wedge
Our pediatrician agreed that this therapist wasn’t right for us, but recommended that we continue until we get the wedge for sleeping as she knew it would help us tremendously with his reflux and breathing while sleeping.
After a delay caused by a large amount of snow, we finally got the wedge. Wow, it made a huge difference. After weeks of struggle, finally we had a solution that helped. Finally H was sleeping. He still snores, sweats, and gasps, but his sleep is so much better.
Otolaryngologist and Initial Scope
In the meantime, we were able to be seen by the otolaryngologist at the children’s hospital. They preformed an endoscopy to confirm the laryngomalacia and severe reflux. The otolaryngologist said that it seemed likely that he was aspirating with eating as the extra tissue from the laryngomalacia covered most of his windpipe and H has had a lot of trouble with eating. For this reason, he did not recommend surgery at this time as it would increase the likelihood of him having more severe swallowing issues in the future. He said this recommendation would be reevaluated as H grows.
He recommended we have a FEES study done to assess how H was swallowing. Depending on what the FEES showed, H might need to be admitted and have an NG tube placed to receive feedings that way until he outgrew the reflux and laryngomalacia and to further observe his eating and breathing.
He told us that all of this will likely get worse and we will need to follow up to see if the recommendation for surgery or and NG tube change or if further tests are needed. He also recommended H have a sleep study done once he is a little order to confirm his sleep apnea (most likely caused by the laryngomalacia).
FEES study
Two days later, we were back at the children’s hospital for the FEES study (fiberoptic endoscopic evaluation of swallowing). This involved H getting a second endoscopy, this time while breastfeeding to see how he was swallowing and if he was aspirating. The scope quickly showed that he was aspirating with even just a very small amount of breast milk. Since H wouldn’t take a bottle, they gave him thickened milk through a syringe to see at what thickness he would be able to drink safely. They established that he could safely swallow nectar thick liquids and we would need to thicken all of his milk to nectar thick or risk aspiration and deep penetration into his lungs.
Thickening His Milk
The team we are working with at the children’s hospital is amazing. The SLP and Occupational Therapist that did the FEES study were able to get him to take a bottle for the first time after the scope was finished. They explained that he probably liked the thickened milk as it made it much easier for him to drink. They also showed me that he needed his check and chin held while he drank the bottle to help with his suck-swallow-breathe coordination. They sent us home with samples of two different thickeners to try (Simply Thick and Gelmix). We would follow up in a week to evaluate how he was doing and if an NG tube would be needed (if he wouldn’t tolerate the bottle).
This meant that I would no longer be able to breastfeed H. I was extremely sad and disappointed to hear that at first. However, realized that I had to do what was best for H. Exclusively pumping my milk has been truly exhausting, time consuming, and emotionally hard. But I am thankful that H is still able to drink my milk and it makes it all worth it.
H was like a different kid. He seemed happy and comfortable for the first time. He wasn’t constantly crying. He wasn’t vomiting and constantly spitting up. He felt good. He was still struggling with the bottle, but he was doing so much better. I finally felt like we had part of the answer.
Silent Reflux and No Weight Gain
Within a day or so it was clear that while he was so much better, he was still struggling. He was still having bad silent reflux (he still had reflux, it just wasn’t coming out as spit up or vomit). His breathing was still constantly labored. He was taking a bottle, but wasn’t eating too much. I also noticed that he was getting a slight developmental delay (he hasn’t smiled yet and was not holding up his head consistently).
His pediatrician doubled his reflux meds and asked the occupational therapist we were seeing for a wedge for playtime hoping it would help him be more comfortable on the flow and in return help with his slight delay.
Occupational Therapy
We had a follow up visit with the feeding therapy team at the children’s hospital a week after his FEES study. The OT noted that he was still struggling with the flow of the bottle (uncoordinated suck-swallow-breathe) and told me to always feed him in an elevated side lying position and to hold his cheek and chin when it seemed like he was struggling. This position would open his airway and help him breath easier while eating. It would also make the flow of the bottle a little slower. She also noted that he still seemed to be struggling with reflux and recommended our pediatrician change us to a stronger reflux medication if possible and refer us to gastroenterology.
He also hadn’t gained any weight in a week and a half. He fell from the 12th percentile to the 7th percentile in weight. She said this was most likely just because he was adjusting to the bottle but we would need a weight check in a week and closely watch it. If it became a trend, he would need to be admitted for an NG tube and possible surgery.
She also set up a second swallow study, this time a VFSS (barium swallow study) for late March to check is swallow and adjust his thickener as needed.
Play Wedge
The Occupational Therapist gave us a play wedge! H immediately loved it! He loves being able to play at his play gym with out struggling to breathe and with reflux. He is also doing wonderful with tummy time and can now hold his head up! A huge change in just a week! L loves it too. It is actually really comfortable for adults too! A week and a half into the play wedge now, and it is still great. However, H has now started coughing a choking while playing on it (we suspect on reflux). He has also had a couple of instances of turning blue after choking while playing on it. His face has also started turning bright red after playing for some time suggesting that he is maybe not moving air effectively for the amount of work his body is doing.
Weight Check and Gastroenterologist Appointment
His weight check was this morning. He has gained just a little weight over the last week and a half. His pediatrician is giving him a little more time to adjust to bottle feeding and recheck his weight. If his weight gain is still slow she wants us to fortify his breast milk with formula to increase his calorie intake. He is still struggling and some days are worse than others. We have his appointment with the pediatric gastroenterologist scheduled for mid March. His pediatrician suspects that they could recommend getting H on an extremely hydrolyzed or amino acid formula (which I would hate). They might also suggest pH monitoring or even a Nissen procedure if he continues to struggle gaining weight.
What’s Next
He will have a third endoscopy and follow up with Otolaryngology at the end of this month to check the progress of the laryngomalacia and see where treatment will go next.
We have noticed that his breathing is getting worse. Especially his choking and coughing after laying on his back (even when elevated 15 degrees). Even a diaper change has caused him to turn blue. His stridor is much more apparent and his retractions are worse. Reflux and sleeping are still areas that we are trying to figure out and he is struggling with.
Chibebe Snuggle Pod
H also was chosen to receive a Chibebe Snuggle Pod from a non-profit that supports families struggling with Laryngomalacia called Coping With Laryngomalacia. It is a wonderful non-profit with an awesome support group that has been so helpful as we navigate this. I was so surprised that H was chosen for the Snuggle Pod! It is essentially a bean bag seat specially made for infants with bad reflux and breathing issues. We are so excited to receive it! It’s coming all the way from Australia, so we are not quite sure when to expect it! Update: we have received it! We are now waiting for the bean filler to arrive so H can try it out!
After weeks of two to three doctors appointments a week, we are happy that this week we have just one! Update: due to slow weight gain we ended up having two… But, we do not have any scheduled for next week, so far.
Although we would like H to be completely comfortable and thriving, we are so happy that at least we seem to be headed down the right track. It’s scary that we haven’t seen the worst yet, but we have a great team for when we do. We are hopefully that H will get over this with no serious troubles and this will all be a distant memory.
This wasn’t my usual newsletter, so I thank you for taking the time to read through what we have been going through. I will keep updating on H and also get back to more Montessori and parenting posts soon!













Ugh, Mama. I am so sorry you guys are going through all of this. It’s a new world to navigate all the medical needs/providers/everything, but feel free to reach out if you have questions or want a sounding or venting board. ❤️
So heart broken. I can't imagine the horror you all are going thru. Wish I could be there with love and Big hugs for you all. In stead I can only send them long distance. Please know that my thoughts and prayers are sent your way. Hang in there H! You have a large family. That lo es you so ery much. Sending ♥️ to you all Alyssia. So proud of you. I'm glad he has you as his mom....